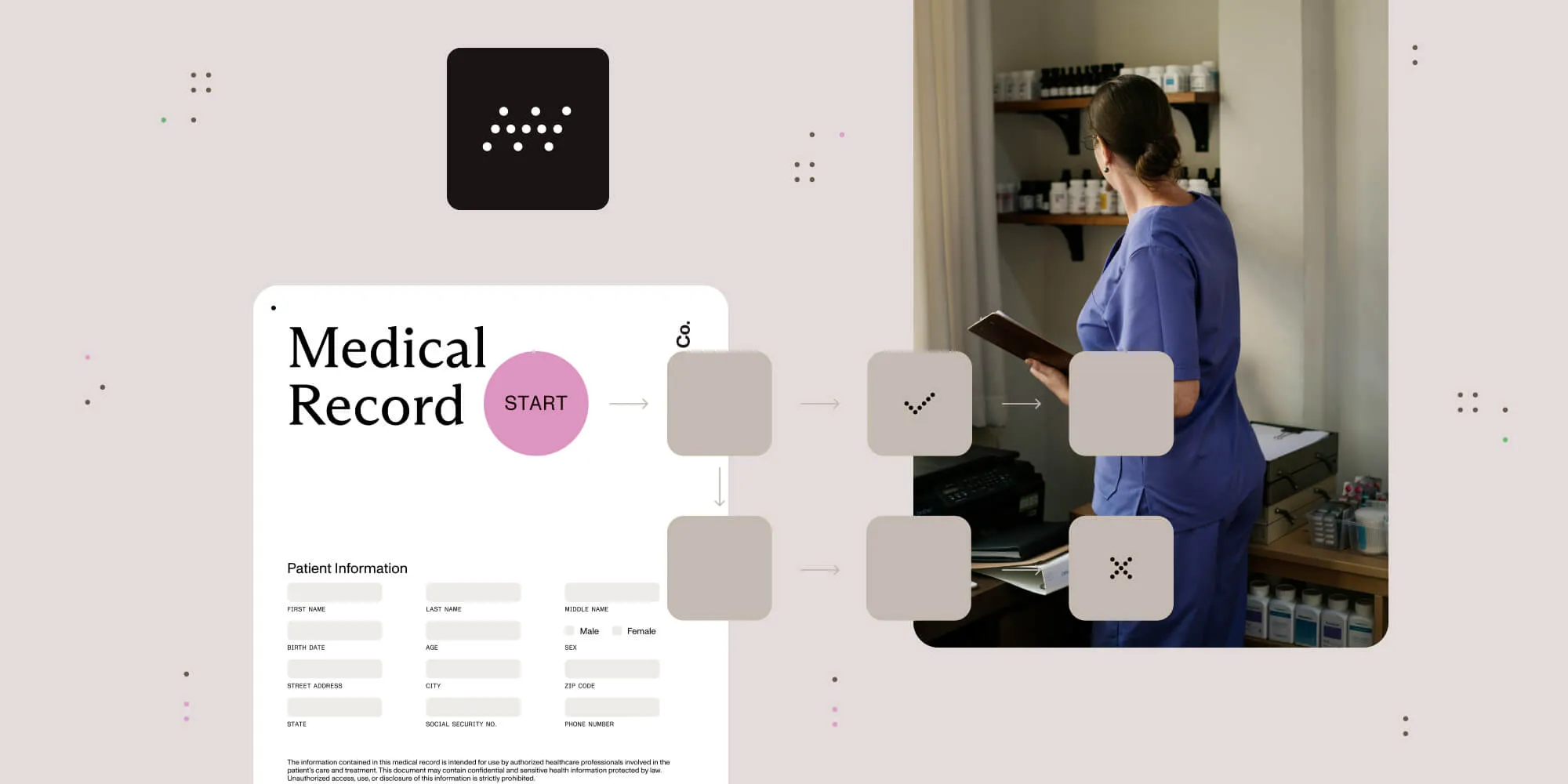
Patient data and healthcare compliance improve with workflow automation
Table of contents
Try Workflow Automation free for 14 days
Effective (and secure!) data management is important across industries, but there are few industries where it’s as important as healthcare. Not only are the stakes high — depending on the situation, accurate and secure patient data management could literally be life or death — but much of the data being managed is considering protected health information (PHI), which adds layers of regulatory complexity and consequences for how the data can be stored, shared, and managed.
Without the right patient data management processes, healthcare providers put both their patients and their practices at risk. But the good news? There’s a way to streamline these processes to not only be more accurate and effective, but also increase compliance at the same time: with healthcare workflow automation.
Modern healthcare organizations are also leveraging document processing automation, digital signature workflows, and compliance management systems to ensure HIPAA adherence while improving operational efficiency.
This article will look at some of the major challenges of managing patient data in the healthcare industry, and show how healthcare workflow automation can help providers and practice managers overcome those challenges and drive improvements across the board.
Challenges of patient data management
However, before covering how healthcare workflow automation can help solve patient data management challenges, it’s a good idea to first outline what those challenges are.
Volume and variety of data
The biggest issue with patient data management in healthcare is the sheer volume and variety of data that needs to be managed.
Healthcare providers collect and maintain a vast variety of information for each patient. For example, a patient file might contain:
- New patient paperwork
- Medical history
- A copy of an insurance card
- Past session notes
- Treatment plans
- Insurance claims
- Billing and payment history
- Patient correspondence
- Correspondence with other providers on the patient’s care team
The list goes on. Each patient has a huge volume and variety of paperwork, and when you multiply that by the number of patients in a practice, you get a ton of data that needs to be managed.
Data accessibility
As mentioned, healthcare organizations generally have a huge variety and volume of patient data to manage. But variety and volume aren’t the only or even the biggest difficulties. The real challenge comes in the form of accessing that data.
Providers are often extremely time-crunched, and they need to be able to access the patient data they need, when they need it. But with so much data to manage, things can quickly become disorganized, especially if the staff is relying on manual workflows — for example, keeping paper files for each patient. Files might get misplaced or stored in the wrong location, or they might be missing key information or documents.
Patient data management software can definitely improve accessibility issues, but it doesn’t necessarily get rid of them completely. For example, if providers or staff members aren’t fully trained on the software, they may not save or store data correctly or be able to access it when they need it. If organizations are using multiple types of practice management software — for example, an electronic health record (EHR), a billing platform, and an appointment manager — and those software tools don’t integrate or “talk” to each other well, it could lead to challenges in accessing data. As an example, you might be logged into one platform but need data from another.
Compliance/regulatory requirements
Patient data is protected under the Health Insurance Portability and Accountability Act (HIPAA), which means healthcare organizations need to comply with all relevant HIPAA regulations that are designed to protect patient information.
We can’t overemphasize the importance of HIPAA compliance. If providers or practices don’t comply, they may find themselves facing hefty fines, disciplinary action, or even legal issues. It’s not just their own data management they have to worry about; if healthcare organizations partner with any vendors or use any software to run their practice, those partners also need to be HIPAA-compliant.
How manual processes amplify patient data management challenges
Clearly, patient data management presents a real challenge to healthcare providers and organizations. But there’s one thing that makes those challenges exponentially harder — using manual processes to manage patient data.
Manual processes — for example, filling out paper records instead of developing medical documentation automation workflows — can cause serious patient data management issues.
Increased risk of human error
It doesn’t matter how smart or competent a provider or staff member is — humans make mistakes. As such, humans manually managing patient data increases the risk of errors, which can end up doing serious harm.
Some examples of potential human errors that could negatively impact a practice and/or patients include:
- Handwriting issues — When a practitioner writes patient notes manually, there’s always the potential that they or other staff members may not be able to accurately decipher what they wrote down. That could lead to inaccurate interpretation or incorrect health information, which can negatively impact the patient’s care.
- Confidentiality issues — When people are manually handling sensitive health information, there’s always a chance that they may inadvertently expose that information to people who aren’t authorized to see it — for example, leaving a patient file open on their desk or on their screen.
- Consistency issues — Different people do things in different ways. When you have multiple people managing patient data, chances are they’re going to manage it inconsistently from one person to the next. This can lead to errors in how data is collected, written, stored, organized, and accessed — inconsistencies that just make running the practice more difficult.
Slower processes
Humans aren’t machines. Relying on manual processes instead of healthcare workflow automation is always going to take longer, which can negatively impact the practice in a variety of ways, including:
- Lowered productivity
- Less time for patient care
- Time loss on tedious tasks
- Potential employee morale issues
- Lower patient capacity
- Less revenue
Compliance challenges
As mentioned, HIPAA compliance is a must in healthcare. But not every provider or healthcare worker is an expert on all things HIPAA. When you rely on workers and providers — instead of on HIPAA compliance tools and software — to manually manage data management processes, there’s an increased risk of noncompliance and all the consequences that go with it, including:
- Unauthorized access of PHI
- Sharing PHI on unsecured platforms, like email
- Issues tracking who accessed what information and when they accessed it
- Miscommunication on compliance practices
Negative patient experience
When processes are handled manually, it causes issues for the patients as well as the practice. Examples of this include:
- Longer wait times during check-in or registration
- Frustration due to incorrect information in records or an inconsistent experience with different providers and staffers
- Violation of privacy or PHI
- Issues with insurance billing or payment
- Communicating and data sharing issues with their larger care team
- Ineffective treatment plans
Financial challenges
All of these challenges often ultimately lead to financial issues within the practice. For example, if claims are submitted incorrectly, it can delay the payout or prevent the practice from getting the full amount it’s owed. Meanwhile, bottlenecks in billing processes lead to slower payment collection from patients. If manual processes cause significant issues within the practice, patients could seek care elsewhere, which will significantly decrease overall revenue for the organization.
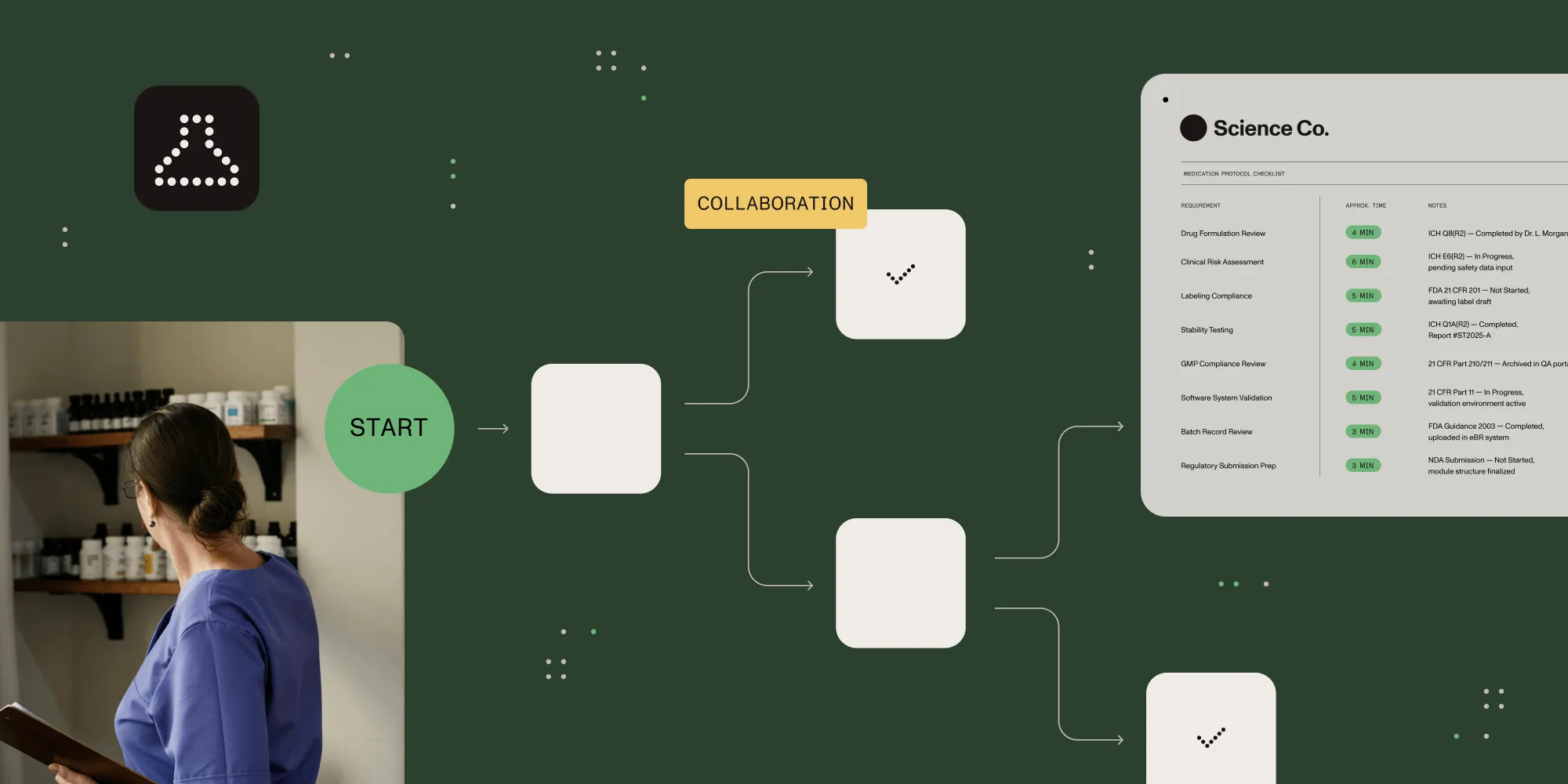
How healthcare workflow automation can streamline patient data management, increase compliance, and improve patient experience
Trying to manage patient data with manual processes not only creates more work for providers and healthcare staffers, but it also lowers efficiency and increases the risk of regulatory issues — which is why moving toward automation is an absolute must.
Automating patient data management processes can improve things for providers, staffers, and patients in a variety of ways.
Create a centralized, digital patient data hub
Instead of having patient information scattered across multiple platforms, paper files, and/or departments, using patient data management software to automate processes creates a centralized digital hub for all patient data. These tools give you the ability to:
- Automate patient data collection with standardized forms and medical document automation
- Store all patient information in one secure, accessible location
- Automatically categorize and organize patient records
- Reduce data entry issues and inconsistencies
- Give providers the ability to easily find the patient information they need
- Ensure compliance with HIPAA and relevant privacy and security regulations
Bottom line? Centralizing your patient data not only makes accessing that data faster and more efficient, but it also creates secure document workflows in healthcare and significantly reduces the risk of lost or misplaced information that’s common with more manual approaches.
Streamline healthcare accounts payable
Healthcare accounts payable (AP) automation can also completely transform the way practices interact with their vendors. Practices can streamline a variety of AP processes, including:
- Digitizing invoice processes
- Automatically tracking invoices from receipt to payment
- Automatically matching invoices with purchase orders (POs) and other relevant documents
- Automatic payment scheduling
- Recording all financial transactions, which can make taxes and auditing more streamlined
- Automatically flagging issues that need review/attention
The impact of all of these automations is faster invoice processing times, significantly fewer errors, and better vendor relationships — which often results in cost savings for the practice.
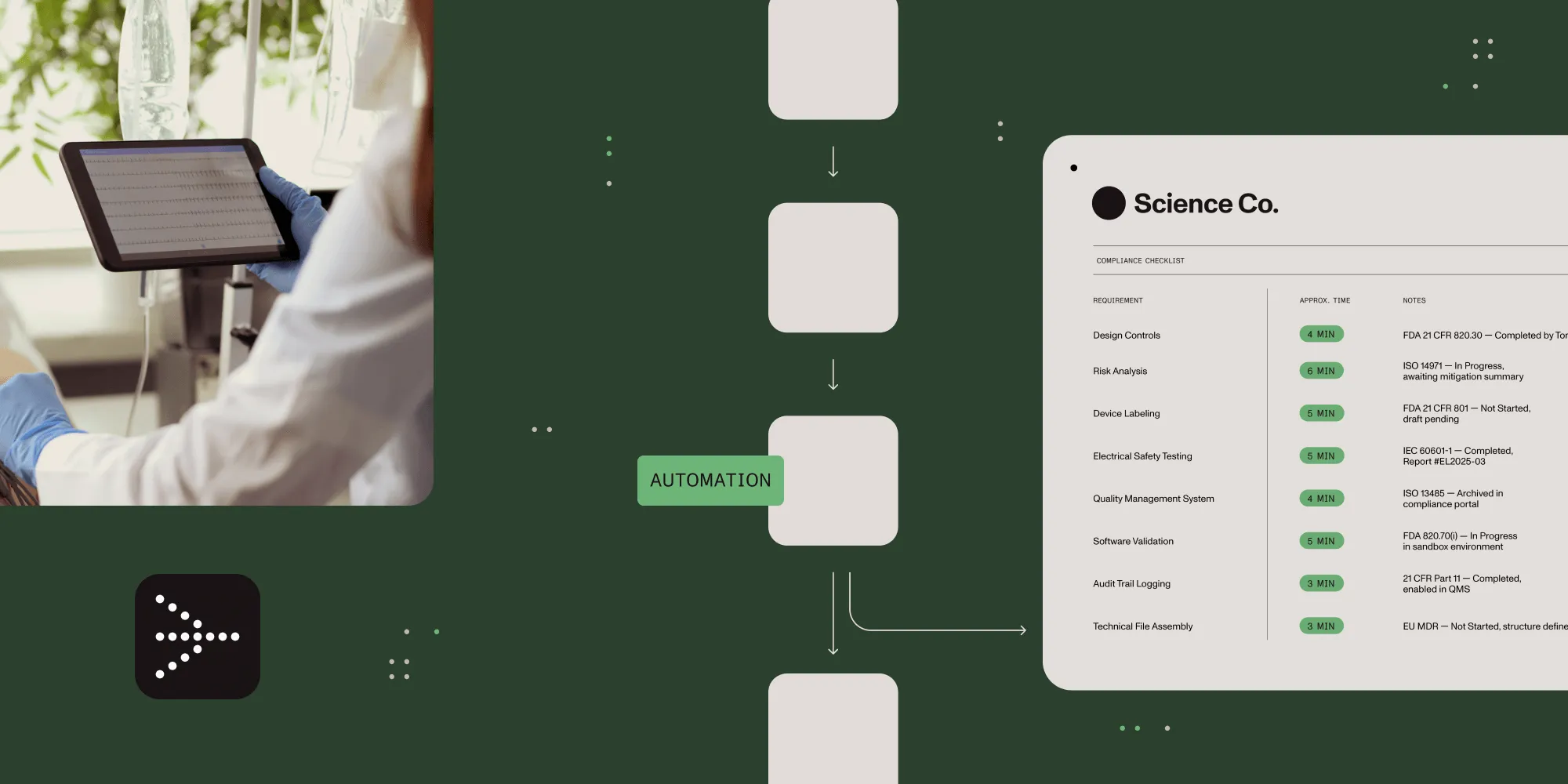
Enhancing compliance and security
Arguably the most critical advantage of workflow automation in healthcare is how it strengthens HIPAA compliance and overall data security:
- Controlled access rights — Automation platforms allow you to set specific permissions for who can access what information, ensuring sensitive patient data is only accessible to those authorized to see it.
- Comprehensive audit trails — Automation software also automatically logs every interaction with patient data — for example, who accessed it, when, and what changes they made — creating a clear documentation trail for auditing and compliance purposes.
- Consistent security protocols — As mentioned, human error is a major security and compliance risk in healthcare. But with automation, instead of relying on staff to remember and apply all relevant security measures, automated workflows build security into the process itself.
- Secure data transmission — Automated systems can ensure that all patient data transfers use encrypted channels, which reduces the risk of data breaches when sharing information (for example, sharing a patient file with another practitioner or corresponding with patients).
At Nutrient, we take security and compliance extremely seriously. We offer access to our assurance reporting via our Trust Center(opens in a new tab), which includes SOC 2 reports that demonstrate how our products achieve key compliance controls and objectives. Our transparency in compliance reporting provides customers with a clear understanding of the controls we’ve established to support operations and compliance.
Improving the patient experience
Workflow automation doesn’t just optimize processes for healthcare providers and staff; it also improves the outcomes and overall experience for patients in the following ways:
- Smoother check-in processes — When the intake and check-in process is automated, patients can fill out forms prior to their appointments, reducing wait times and minimizing day-of paperwork.
- Less repeats of information — When patient data is properly stored and accessible, patients don’t need to repeat their medical history or insurance information to multiple staff members across multiple visits, saving both time and frustration.
- Better care coordination — Automated workflows allow providers to easily share and access information from and with other practitioners on the patient’s care team, leading to a more cohesive care experience.
- More face time with providers — When administrative tasks are automated, healthcare providers are able to spend more time with patients and less time on paperwork.
- Improved communication — Things like automated appointment reminders, follow-up instructions, and secure messaging capabilities improve patient-to-provider communication, and improve the patient experience in the process.
By streamlining and automating these critical patient-facing processes, healthcare organizations can significantly enhance patient satisfaction while simultaneously improving operational efficiency. This not only leads to better health outcomes but also strengthens the practice’s reputation in the community. The result is a more sustainable, successful healthcare operation that better serves both patients and providers.
Interested in learning how healthcare workflow automation can work for you? Check out our free trial, or contact Sales for a demo!